Presenting the facts: breast cancer in young women
August 28, 2023
Breast cancer in the primary care setting
Breast cancer management, particularly for young women, is an intricate process that demands the collaboration of a multidisciplinary team. A General Practitioner who is informed about this complex course can provide optimal patient care. Understanding the treatment pathway, including egg harvesting/freezing for fertility preservation, surgery options, and the role of medical oncology, radiation oncology, geneticists, and Breast Care Nurses is crucial. This helps GPs guide patients smoothly through the healthcare system, ensuring they receive timely and appropriate interventions and support.
Recognizing the indications for genetic testing in young breast cancer patients is also vital. Certain genetic mutations (like BRCA1 and BRCA2) can dramatically increase breast cancer risk, and identifying these can direct treatment decisions, inform risk for relatives, and guide prophylactic measures. An informed GP can help a patient understand the testing process, potential results, and their implications. A GP should also understand the benefits of neoadjuvant chemotherapy and immunotherapy. These treatment modalities can shrink tumours prior to surgery, potentially making breast-conserving surgery possible, and can also provide early indications of how the cancer is responding to the treatment. This can help in explaining treatment plans and their potential impacts effectively to patients.
With identification and diagnosis of breast cancer an upward trend, GPs will continue to play a key role in managing side effects of treatments including radiation, chemotherapy, and immunotherapy. These treatments can have a range of side effects, from fatigue and nausea to more serious complications like immune-related adverse events. By understanding these side effects, primary care can promptly recognize and address them, ensuring the patient’s comfort and safety and reducing time spent in hospitals during this testing period.
Breast Cancer and young women
For over half a century, Ramsay Health Care has been committed to its guiding principle of ‘People Caring for People’, extending this dedication to encompass the detection, management, and recuperation from cancer Australia-wide. They provide high-quality, individualised, and comprehensive care, guaranteeing patients can access specialised care wherever and whenever they require it in a private setting.
Thanks to individualised treatment strategies, proficient medical teams, and a nationwide interconnected care network, Ramsay Cancer Care paves the way for integrated medical, clinical, and supportive care around the country. Hosted by Ramsay Health Care, Breast Cancer and Young Women is a comprehensive online workshop, specially curated to delve into the advanced aspects of managing breast cancer in young women. These modules presented in 1 easy pre-recorded format are presented by leading experts, offering invaluable insights into the latest developments in breast cancer treatment strategies.
Dr Eva Nagy
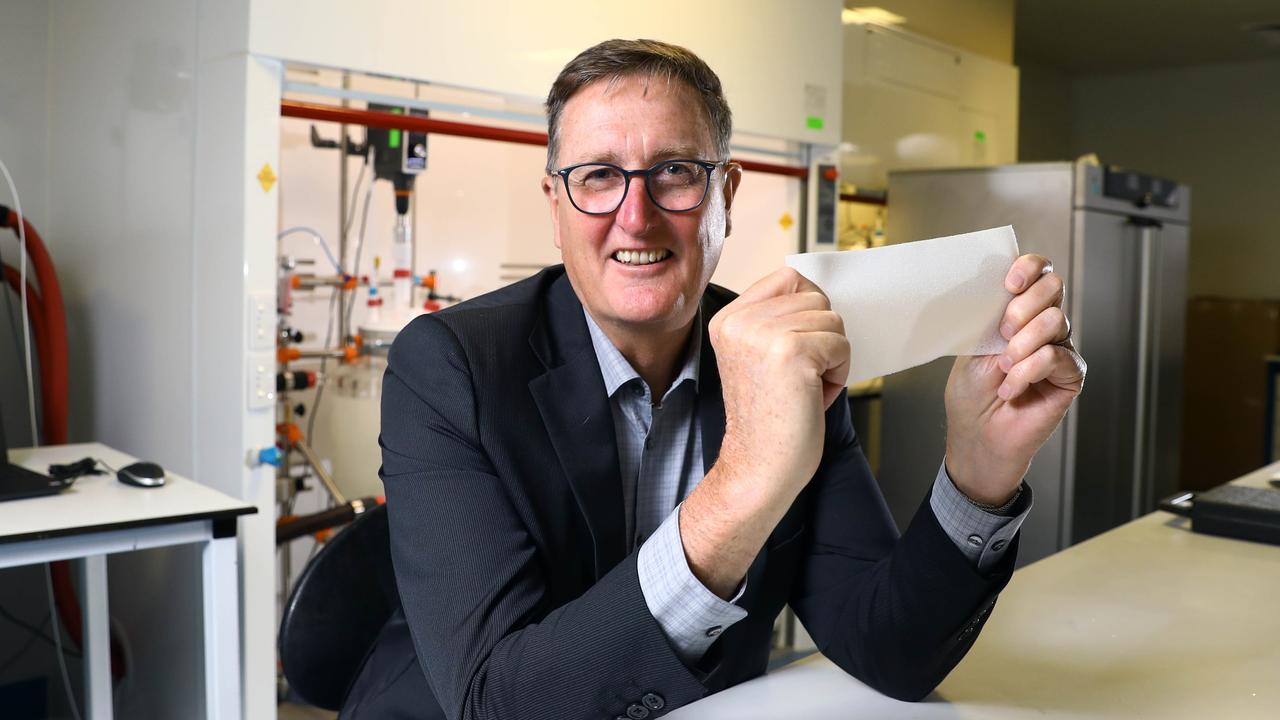
Dr Nagy, a Consultant Breast Surgeon at Sydney Oncoplastic Surgery, has had an extensive medical career spanning Melbourne, Singapore, and Sydney. A graduate of the University of Melbourne, she undertook formal surgical training at institutions including the Royal North Shore Hospital and St. Vincent’s Hospital. She specialised in Breast Surgery at the Poche Centre in North Sydney and the Nottingham Breast Institute in the UK, where she gained proficiency in advanced surgical techniques and reconstructive options.
Dr Nagy has a deep interest in promoting breast-conserving surgery (lumpectomy) and reconstructive techniques to optimise patient quality of life and appearance post-surgery. Her research efforts focus on the potential for safely de-escalating treatment protocols in cancer care.
Dr Nagy has contributed to educational resources for both professionals and the public, including Cancer Council Australia’s Understanding Breast Cancer brochure and North Shore Private Hospital’s GP Updates. She holds an MBBS, a PhD in Biomedical Science, a Bachelor’s Degree (Hons) in Biomedical Science, and a Graduate Certificate in Breast Surgery from the University of Sydney. She is a member of Breast Surgeons of Australia and New Zealand and Breast Cancer Trials, and a Visiting Medical Officer with BreastScreen NSW.
Dr Sally Baron-Hay
Dr Sally Baron-Hay, MBBS FRACP, is a seasoned medical oncologist with over 20 years of clinical experience and a senior lecturer at the University of Sydney. She holds clinical appointments at the Royal North Shore Hospital, North Shore Private Hospital, The Mater Hospital, and Genesis Care in Sydney.
After completing her undergraduate training at the University of Western Australia and Sir Charles Gairdner Hospital, she further developed her interest in translational oncology clinical trials at the Royal Marsden Cancer Centre in London. Her medical oncology training continued at RNSH and Royal Prince Alfred Hospital. At the Kolling Institute, she researched the role of Insulin Like Growth Factors in ovarian cancer pathogenesis, winning the AACR Young Cancer Investigator award and a NHMRC Scholarship for her work.
Dr Baron-Hay focuses on clinical research into breast and gynaecological cancers and participates in the Ovarian Cancer working tumour group within the Australian New Zealand Gynae Oncology Group. She’s instrumental in formulating guidelines for patient care during and post-cancer treatment. As an advanced trainee supervisor at RNSH, she mentors future medical oncologists. She also contributes to the eviQ Medical Oncology Reference Committee for treatment protocols. Her current clinical interests lie in enhancing outcomes for women with breast and gynaecological malignancies through personalised treatments.
4 Modules to ensure better patient outcomes
De-escalation of Surgery and Preservation of Breast and Axillary Nodes in Young Women with Breast Cancer is led by Dr Eva Nagy. Lead by renowned Breast Surgeon, Dr Nagy talks through the focus on modern surgical approaches, which aim to decrease the invasiveness and extent of surgical procedures while preserving the breast and axillary lymph nodes. These strategies minimise the physical and psychological impacts of surgery, while still prioritising optimal oncological outcomes.
The Role of Neoadjuvant Chemotherapy and Immunotherapy in Young Women’s Breast Cancer by Dr Sally Baron-Hay, a leading medical oncologist, elaborates on the evolving roles of neoadjuvant chemotherapy and immunotherapy in young women’s breast cancer management. These pre-surgery treatments can downsize the tumour, potentially allow for breast-conserving surgery, and help gauge the effectiveness of the therapeutic regimen, guiding further treatment decisions.
Genetic Testing for Young Women with Breast Cancer: BRCA and Beyond is presented by Dr Mathilda Wilding. Dr Wilding guides you through the intricacies of genetic testing for young women with breast cancer. While BRCA mutations are well-known, the discussion expands to include other significant genetic factors, outlining the implications of these genetic alterations on treatment decisions, risk management, and familial implications.
Lastly, Radiotherapy Treatments – Adjuvant vs Reverse Sequencing by Dr Marita Morgia, illuminates the nuances of radiotherapy in young women’s breast cancer management. The course explores the classic adjuvant approach versus reverse sequencing, examining the benefits and implications of both to help inform personalised treatment strategies.
Find this course via https://app.medcpd.com/courses/3224