The Ban on Denying Insurance Based On Genetic Testing
November 25, 2024
Patient’s Rights Restored
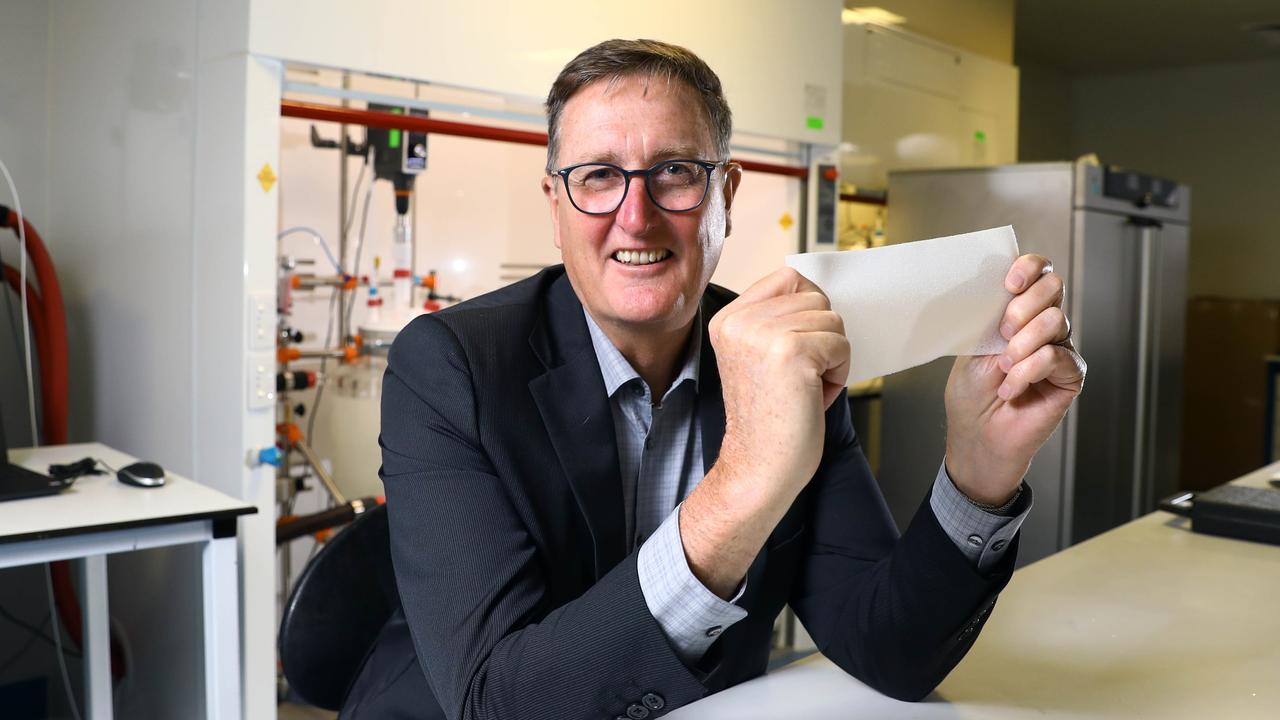
The recent government decision to ban life insurers from using genetic testing as grounds for denying coverage or increasing premiums marks a profound shift in healthcare and insurance policy in Australia. For medical professionals, this regulatory change raises critical questions about ethics, patient autonomy, and the broader implications of genetic testing in clinical and commercial contexts. While proponents see this decision as a protective step towards patient rights and ethical integrity, others worry it may cloud the landscape of risk assessment and resource allocation.
For healthcare providers, genetic testing is an increasingly valuable tool, not just in diagnostics but in enabling preventive care and guiding treatment plans. Yet, as this ban suggests, the social implications of genetic information extend beyond medical benefits. Will this regulatory shift will serve patients’ best interests in the long run – and invite an open discussion on the role of genetic information in both healthcare and financial security?
The Impetus Behind the Ban
A significant deterrent to genetic testing has been the fear that such information could be used against individuals by insurers, particularly in life and disability coverage. Many Australians, aware of family histories involving inherited diseases, are hesitant to undergo genetic testing, even if it could offer life-saving insights. The potential misuse of this information in policy evaluations led to calls for a ban, which culminated in the government’s recent decision.
The hope is that this policy reform will remove barriers to genetic testing and encourage people to pursue critical health evaluations when necessary, without fearing the financial repercussions. In the wake of these changes, we are likely to see a surge in genetic testing and referrals to seek familial answers and predictions. From the perspective of healthcare providers, will this ultimately enhance patient health outcomes? Or do we risk encouraging genetic testing without fully preparing patients for the psychological and medical implications of such knowledge?
Lessons from Abroad
Looking beyond our borders for answers to these important questions, countries such as Canada and the United Kingdom have long upheld similar restrictions, with the aim of preventing discrimination based on genetic predisposition. In these nations, the primary goal has been to establish a healthcare-first approach, ensuring patients’ genetic data serves them within the clinical context without carrying over into their financial affairs.
There’s merit in these precedents; however, implementing them within a different healthcare structure may lead to unique challenges. While this ban will certainly have significant impacts on patients, it also raises questions about the scope and transparency of health insurance policies — of which we known to be fraught with clauses and exclusions.
Resource Allocation
Life insurance, by its nature, is a product built on risk assessment. Historically, insurers have relied on family history and personal medical records to gauge future health risks. With genetic testing, there was potential for a more granular understanding of individual predispositions. However, critics argue that this more precise data could become a tool for denying coverage to those who may need it most.
This move also hints at a deeper ethical consideration. If genetic testing becomes more widely used and relied upon in clinical practice, do we inadvertently set a precedent where every health issue must be backed by genetic validation? For some conditions, a genetic predisposition might be helpful; for others, it could complicate care and burden patients with data that may have limited practical use. How will this trend affect our clinical judgement and the way we communicate risk to our patients?
Advocates and Educators
With these changes now in place, healthcare professionals are at the forefront of helping patients understand the implications of genetic testing, both medically and financially. This may require additional conversations in clinical settings, and advocacy for qualified geneticists with genetic counselling techniques, where patients can ask questions about the benefits and limitations of genetic insights. Providers can also become advocates, encouraging transparency in insurance policies and fostering public discourse on the value of genetic data within medical contexts.
The recent ban is undeniably a step forward for patient rights, but it is only one piece of a larger puzzle. For medical professionals, the ethical and practical challenges presented by this regulation mean that we must adapt our roles as both clinicians and educators. It also poses a significant opportunity to actively participate in shaping how these policies will be reviewed and possibly revised in the future.
The full press release is available here – https://ministers.treasury.gov.au/ministers/stephen-jones-2022/media-releases/total-ban-use-adverse-genetic-testing-results-life