The First Case of Lung Transplantation for COVID‐19 in Australia
March 19, 2025
Lung Health Following COVID-19
Research over the past few years has made it clear that while many individuals recovered well from COVID-19, a notable subset may continue to experience respiratory issues. In some cases, lung damage can be so severe that it leaves survivors with persistent or even permanent scarring.
In the early stages of the pandemic (2020–2021), clinical observations suggested that a portion of those who survived COVID-19 did not regain their usual lung capacity. Follow-up research from China and Europe revealed significant residual lung abnormalities at three to six months post-infection. An early cohort in Wuhan found that most hospitalised survivors continued to display CT opacities and impaired diffusion capacity at six months. A similar study from the UK reported that around half of those hospitalised with COVID-19 felt they had not fully recovered even a year after discharge. By mid-2020, case reports began to appear describing post-COVID pulmonary fibrosis—a chronic, scarring process that had been seen in severe, Acute Respiratory Distress Syndrome(ARDS)-like cases. In the most advanced scenarios, lung transplantation was considered or performed to save patients whose lung tissue had been irreversibly damaged, a therapeutic approach previously used for end-stage ARDS.
Longitudinal Data
As larger studies emerged in 2022–2023, a more detailed perspective took shape. A meta-analysis of approximately 2,000 patients found that around 45% of recovered COVID-19 cases showed radiographic evidence of fibrosis. Those who developed lung fibrosis generally had more severe acute illness, requiring ICU care, lengthy hospital stays, or presenting with high inflammatory markers. Chronic symptoms in fibrotic patients included dyspnea, cough, chest discomfort, fatigue, and muscle weakness, nevertheless, many reports indicated a pattern of partial recovery over time. A two-year study revealed that the percentage of survivors with any persistent symptom dropped from 68% at six months to 55% at two years, suggesting that mild scarring or ground-glass changes may regress if they are not well established. For individuals with extensive fibrotic patterns, such as honeycombing or significant reticulation, these changes often prove permanent.
Australia’s experience differs somewhat from regions that witnessed large case volumes early in the pandemic. Strict containment measures in 2020 meant fewer serious infections initially, but some unvaccinated individuals with severe disease later presented with lasting pulmonary complications. By late 2021–2022, higher vaccination rates and milder Omicron variants led to many more overall infections but fewer critical lung injuries. Even so, Australian surveys estimate that 5–10% of individuals infected with COVID-19 continue to have symptoms for at least three months, though only a fraction of them develop true organ-level damage. At a Melbourne post-COVID clinic, 13% of patients reporting long COVID symptoms between 2020 and 2022 required specialty respiratory care. Current evidence shows that chronic lung impairment remains one of the more serious consequences of COVID-19 in a small yet significant group of survivors.
Irreversible Lung Damage
For those whose COVID-related fibrotic changes become permanent, there is no definitive cure at present. Treatment emphasises preventing further decline and enhancing quality of life, as recommended by both Australian and international guidelines. A comprehensive approach typically integrates rehabilitation, careful medical oversight, and lifestyle modification. In 2023, the nation witnessed its first lung transplant specifically for COVID-19-related pulmonary fibrosis. This landmark case saved a life while challenging our healthcare system to establish clear protocols and best practices for patients with severe post-COVID respiratory failure.
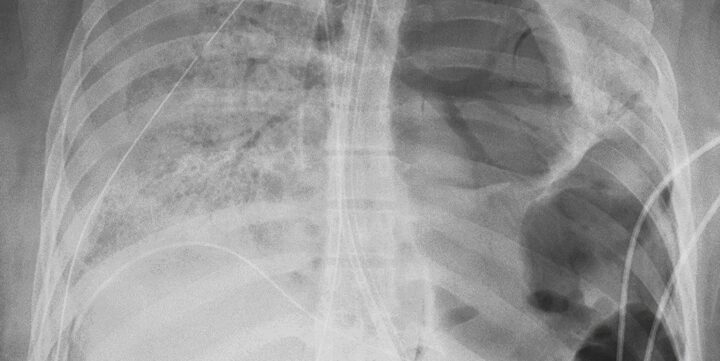
The patient at the centre of this milestone was a 61-year-old man with only mild asthma in his history and minimal past smoking. After contracting COVID-19 in December 2022, he deteriorated rapidly, progressing from mild coryzal symptoms to acute type 1 respiratory failure in five days. Despite optimal medical management, including antibiotics, antifungals, baricitinib, remdesivir, and dexamethasone, he required prolonged veno-venous extracorporeal membrane oxygenation (ECMO). When repeated attempts at weaning failed, imaging demonstrated advanced fibrotic changes, rendering transplant the only curative option.
Multiple complications arose, including high HLA sensitisation following platelet transfusions and a chronic-phase Chagas disease detected on nucleic acid testing. Despite these hurdles, the patient underwent a successful bilateral lung transplant six months after admission, was discharged oxygen-free 20 days later, and remains functionally independent. This remarkable journey highlights how even in the face of formidable barriers, modern therapies can transform patients.
The broader reality of post-COVID lung disease is increasingly apparent. Many individuals who survive severe COVID-19 display persistent or progressive lung injury, sometimes resulting in disabling dyspnoea and other symptoms long after acute recovery. Pulmonary function tests often reveal a reduced diffusion capacity; in the most severe cases, a restrictive ventilatory pattern emerges. While conservative measures are usually effective in stabilising or improving lung function — including pulmonary rehabilitation, careful oxygen therapy, and vigilance against secondary infections — some patients continue to deteriorate.
In such situations, ECMO can serve as an essential bridge to lung transplantation. If the patient remains incapable of sustaining oxygenation or ventilation with conventional measures, and if repeated imaging confirms no improvement in lung compliance or gas exchange, the possibility of permanent lung damage demands serious consideration of transplant. According to international guidance, transplant candidates typically must show no signs of recovery for a sustained period, possess negative COVID-19 tests, and have no other comorbidities precluding surgery. Research suggests that short- and medium-term outcomes of COVID-19 lung transplant recipients are at least comparable to those of other transplant cohorts. In many programs worldwide, ECMO is deployed with the goal of maintaining patients long enough for them to recover from systemic complications while they await suitable donor lungs.
Australian Outcomes
In Australia’s experience, the recent Victorian transplant has illuminated how complex such cases can be. The patient’s high HLA sensitisation and chronic Chagas disease required meticulous planning and considerable delays. Even so, the procedure itself proceeded successfully, and the patient’s progress at follow-up demonstrates how meaningful such an intervention can be for those who have no remaining alternatives. As more data accumulates, it will be important to refine patient selection and timing. Clinical research and long-term registries will help determine survival rates and potential challenges, such as graft rejection, infections, and respiratory complications.
The Australian experience thus far underscores the importance of thorough assessment and early identification of patients at risk. Post-COVID care pathways should remain vigilant for those with severe or lingering symptoms, facilitating timely investigations and ensuring a clear pipeline to advanced therapies when standard treatment fails. The hope is that for most patients, pulmonary rehabilitation, infection control, and optimal medical management will be sufficient to arrest or reverse lung injury. For the unfortunate few whose lungs remain irreversibly damaged, transplantation offers not just prolonged survival but often a chance for renewed independence and meaningful quality of life.
Farghaly S, Badedi M, Ibrahim R, et al. Clinical characteristics and outcomes of post-COVID-19 pulmonary fibrosis: A case-control study. Medicine (Baltimore). 2022;101(3):e28639. doi:10.1097/MD.0000000000028639
Hama Amin BJ, Kakamad FH, Ahmed GS, et al. Post COVID-19 pulmonary fibrosis; a meta-analysis study. Ann Med Surg (Lond). 2022;77:103590. doi:10.1016/j.amsu.2022.103590
Wong M, Gardiner B, Stirling R, et al. Putting international practice into action: the first case of lung transplantation for COVID-19 in Victoria, Australia. Med J Aust. 2025;222(4):179-180. doi:10.5694/mja2.52597